- Für Dienstleister
- Für Makler
Einzelpersonen und Familien
Wen wir abdecken
- Im Ausland lebende Personen
- Familien
- Studenten
- Arbeiten im Ausland
- Rentner
- Über 60 Jahre
Top-Ziele, die wir abdecken
Krankenversicherung für Expats
- Wissenswertes zur Gesundheit von Expats im Hub
- Übersicht für Rentner zur internationalen Krankenversicherung
- Eine Übersicht zur internationalen Krankenversicherung für die Arbeit im Ausland
- Krankenversicherung für Expats im Detail
- Übersicht für Studenten zur internationalen Krankenversicherung
- Umzug ins Ausland während der Schwangerschaft
Krankenversicherung wählen
- Reiseversicherung oder internationale Krankenversicherung
- Krankenversicherung wählen
Länderratgeber
- Länderratgeber
FAQ
- Häufig gestellte Fragen
Arbeitgeber
Global Health Benefits Europa
- Krankenversicherungen für Arbeitgeber
- Cigna Inspire Versicherung
2 bis 149 Mitarbeiter
- Internationale Krankenversicherungen
Große Unternehmen
- Krankenversicherungen für große Unternehmen
IGO/NGO und Behörden
Themen
Einzelpersonen und Familien
-
Versicherungsschutzarten
-
Wo wir abdecken
- Argentinien
- Australien
- Österreich
- Brasilien
- Kanada
- Chile
- China
- Costa Rica
- Ägypten
- Frankreich
- Deutschland
- Griechenland
- Indien
- Indonesien
- Irland
- Italien
- Japan
- Kuwait
- Mexiko
- Niederlande
- Philippinen
- Portugal
- Singapur
- Südafrika
- Spanien
- Schweden
- Schweiz
- Thailand
- Türkei
- VAE
- Vereinigtes Königreich
- USA
- Vietnam
-
Ressourcen
- Wissenswertes zur Gesundheit von Expats im Hub
- Übersicht für Rentner zur internationalen Krankenversicherung
- Eine Übersicht zur internationalen Krankenversicherung für die Arbeit im Ausland
- Krankenversicherung für Expats im Detail
- Übersicht für Studenten zur internationalen Krankenversicherung
- Umzug ins Ausland während der Schwangerschaft
- Reiseversicherung oder internationale Krankenversicherung
- Krankenversicherung wählen
- Länderratgeber
- Häufig gestellte Fragen
-
Für Mitglieder
Arbeitgeber
-
Unsere Versicherungen
-
Für Mitglieder
IGO/NGO und Behörden
- Übersicht
-
Unsere Versicherungen
-
Für Mitglieder
Blog zum Thema Gesundheit
Für Makler
Let's Talk About the Relationship Between Mental and Physical Health
Let's Talk About the Relationship Between Mental and Physical Health
With stress being the root cause of many serious and life-altering conditions, it’s important we talk frankly about how our mental health affects our physical well-being, writes Dawn Soo, Medical Director, Asia, Middle East & Africa at Cigna Healthcare.
Over my 20-year career as a medical officer and practitioner, I’ve observed few health conditions wreak as much far-reaching damage on patient well-being and quality of life as stress.
Six in 10 of us experience high levels of stress, and young people tend to feel it worse. In fact, Cigna Healthcare’s latest assessment of global well-being shows how today’s main driver of stress – the cost-of-living crisis – is having an unprecedented and disproportionate impact on younger generations.
The consequences of this global state of mind are worrying. Earlier onset of chronic disease, a greater burden of physical illness, and in the most severe cases, premature death. It’s a troubling fact that people with mental illnesses live anywhere between 10 to 20 years less than those without.
In light of these facts, there can be little doubt that stress and its toll on our bodies is one of the world’s most pressing health issues. Let’s talk about it.
The Relationship Between Mental Health and Physical Health
A few years ago, I embarked on a research project exploring the connection between mental health and physical illnesses. We wanted to understand if individuals with pre-existing mental health issues would face more significant challenges when dealing with a physical ailment, and whether they would require extra support to return to good health from major treatment or ill-health, like hip surgery or pneumonia.
It’s well known that many, if not all physical health problems come with a psychological dimension, and those who suffer long-term physical health conditions are susceptible to severe mental health problems, such as depression or anxiety.
But our task was the opposite: to quantify the financial impact so that people could really appreciate the link between mental ill-health and general physical well-being. That is, how investing in mental health benefits can help to counteract physical ailments.
The results of our study were surprising. Despite appreciating the significant economic toll of mental ill-health on physical productivity, many companies and HR departments still struggled to grasp the interconnectedness of the two elements of well-being. Instead, they tended to treat mental health as a separate issue, overlooking its influence on physical health.
The conclusions were obvious: addressing mental health alongside physical conditions is crucial. For example, treating a work-related back injury will require physiotherapy but may also necessitate counselling services, via health insurance or benefits packages, to treat the underlying stress or tension contributing to the orthopedic or muscular strain.
Stress: The Misunderstood Link Between Mental and Physical Health
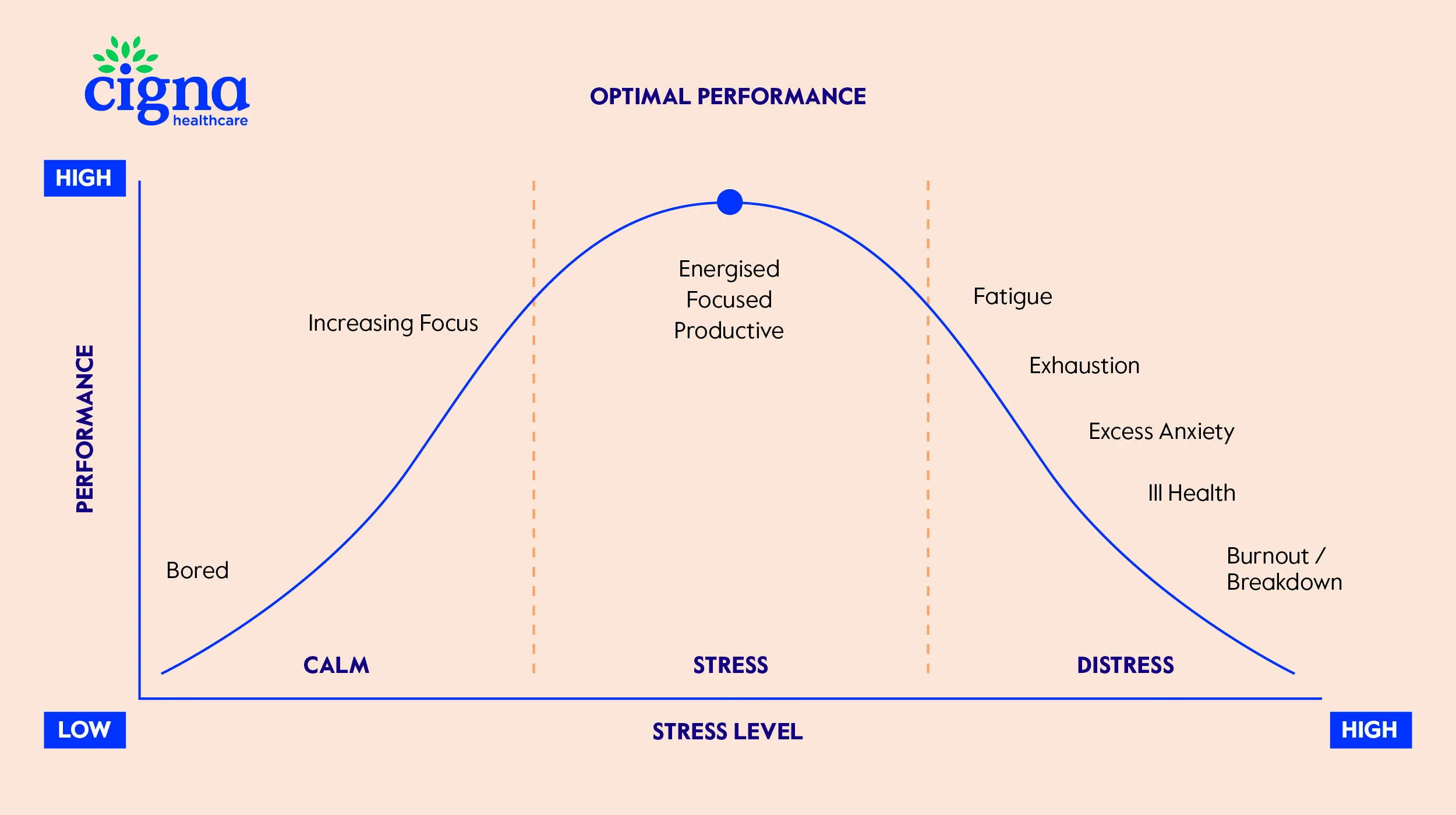
Stress is both a global problem and a fundamental part of life, for better and worse. A small amount of acute stress is to be expected and can even be good, as it helps us with decision-making and performing daily activities. The trouble starts when stress persists.
Too much or chronic stress can overwhelm our mind and body, causing a number of physical health issues, from increased vulnerability to viral infections, to headaches, fatigue, insomnia, overeating, and gastrointestinal problems. It also leads to life-threatening conditions, such as hypertension, heart disease, Type II diabetes, obesity and metabolic syndrome, as well as a heightened risk of substance abuse.
Although the link between stress and overall physical well-being may be obvious to healthcare professionals, patients often neglect symptoms or delay diagnosis due to fundamental misconceptions about the nature of stress and mental health.
In many instances, people first try to cure the physical symptoms, without recognizing the social or personal determinants of stress as the root cause. For example, a patient may go for dozens of physiotherapy sessions to treat their back pain and achieve limited relief as they have not acknowledged their pain as induced by work or social or cultural stressors.
But the consequences of our collective inability to talk about stress early are felt by all.
It’s estimated that chronic stress causes much greater health service utilisation, more visits to the family doctor, counsellor, specialists and hospitals, exacerbating the already huge demand on our healthcare systems.
The demand that physical ailments inevitably place on health providers due to untreated underlying psychological conditions is an issue that companies like Cigna Healthcare are constantly seeking to address through better, more preventative and holistic well-being benefits.
Chronic inflammation: How Physical Health Conditions Affect Mental Health
In 2019, my research explored the correlation between common physical illnesses and mental health. Specifically, we identified connections between conditions like eating disorders and chronic gastritis, which are both linked to chronic inflammation. This inflammation, often triggered by an unhealthy diet, lack of exercise or chronic stress, not only heightens the risks of diabetes and obesity but also acts as a defense against infections and injuries.
Interestingly, however, recent years have revealed a twist in our understanding of inflammation. Rather than just serving a protective purpose, we now know that inflammation plays a role in the genesis of certain types of depression.
Notably, individuals grappling with inflammatory ailments tend to be more susceptible to depression than those dealing with non-inflammatory conditions like heart disease. This susceptibility escalates alongside the level of inflammation, then amplifying the risk of depression in a vicious cycle.
Appreciating inflammation's complex duality – acting as both a protector and a potential underminer of our mental health – is going to be increasingly crucial to our collective understanding of how physical health and mental well-being are intricately linked and play equal roles in holistic well-being.
How can I approach my health holistically?
Here are a few key habits that will help you stay on top of your mental and physical health:
- See your doctor: This may be challenging for some, as recent years have made it harder to keep up sustainable and preventable treatment despite increasing awareness about stress and mental health. During COVID-19, regular GP and family doctor visits fell disastrously, and in the wake of the pandemic we have seen issues with access and affordability. Nevertheless, seeing a doctor regularly is vital.
In acutely stressful situations, up to six sessions with a mental health professional or specialist clinician might be enough for you to cope better and get on top of any emerging physical issues. But if you’re experiencing chronic stress over an extended period, you will likely need more systematic support.
- Manage your working hours: With today’s ‘always on’ culture it’s incredibly easy for work to dominate every waking hour. In a study last year, we found that nearly all employees globally were showing signs of burnout, a major cause of mental ill-health, which can manifest itself physically as back pain or other conditions. While everyone’s working style is different, it’s important to manage your boundaries between work and personal time.
- Practice Mindfulness: Dr. Stella George, Chief Medical Officer, Cigna International is a great exponent of the value of breathwork, which along with meditation, yoga, or any number of other practices can assist you in connecting to your body and quieting your mind, allowing you to become more grounded and calm.
- Speak to your family and friends: In 2020, around 78% of people globally who suffered anxiety or depression actively turned to family or friends to talk about their condition, leaving a significant shortfall of people across the globe who stayed silent.
The value of talking openly about our mental health cannot be understated, and our first port of call is usually our family and friends.
- Stay active: The role physical exercise plays in supporting a healthy mind and body is becoming more and more apparent. Movement helps keep you balanced and in shape – both in mind, body and mood.
Looking towards a new approach to holistic and preventative healthcare
The connections between mental and physical health are undeniable and profound.
Chronic stress and mental illnesses silently impose a heavy toll on physical well-being, costing trillions to the global economy and stealing precious years of life from billions of people.
Promisingly, however, the interplay between mental and physical health has gone from being an obscure corner of research to a central field of medical attention and even popular awareness. And as I look to the future of medicine, it is exciting to see the mind-body connection emerging as the next significant area of discovery for effective, holistic, and preventative healthcare.

But, for this knowledge to improve our everyday quality of life, it is essential that we pay attention to how stress, inflammation, exercise, sleep, diet, and social connections all interact, and that patients and clinicians pursue holistic healthcare strategies that reflect this link.
Of course, one of the most important elements of this new approach will be our ability to talk openly with our doctors, friends, and family about how we are doing physically, mentally holistically. Be brave and ask someone you know how they are doing emotionally or share your recent emotional state to start a conversation. As Dr. Aratow suggests, “Language is a powerful force, and we have to get to a point where the word ‘health’ means both physical and mental well-being, and when we are there, the stigma fades away and the tides can be turned on the decades long mental health epidemic affecting the entire world.”
Verwandte Artikel
@Cigna 2025
This article serves only as a reference and is intended for informational purposes only. Nothing in this article constitutes legal, tax, financial planning, health or medical advice including diagnosis or treatment. Any reference to products or services offered by Cigna are available except where prohibited by applicable law and subject to terms and conditions. Cigna have no involvement in, nor are we liable for, any decisions and/or outcomes that are made or determined by FocusPoint International.
Kontakt
Hier finden Sie die richtige Information - Von unsrer Verkausfabteilung bis zu generellen Information, einschließlich Kontaktinfromatinon für existierende Cigna Kunden.
KontaktinformationenBeliebte Links
Ressourcen
© 2025 Cigna Healthcare. Alle Rechte vorbehalten.
* Bitte beachten Sie, dass dies eine Darstellung der verfügbaren Leistungen ist und die für jede Leistung geltenden spezifischen Bedingungen und Ausschlüsse hier nicht enthalten sind. Die Leistungen können geändert werden. Einige Leistungen sind Teil des optionalen Moduls. Ausführliche Informationen finden Sie im Kundenleitfaden.
Diese Website wird zur Verfügung gestellt von Cigna European Services (UK) Limited, einem in England und Wales eingetragenen Unternehmen mit Sitz 13th Floor, 5 Aldermanbury Square, London EC2V 7HR und Registernummer 00199739. Der Name und das Logo von Cigna Healthcare sowie andere Cigna Healthcare Marken sind Eigentum von Cigna Intellectual Property, Inc. und für die Verwendung durch die Cigna Group und ihre operativen Niederlassungen lizenziert.
Bei der Auswahl dieser Links verlassen Sie Cignaglobal.com. Cigna Healthcare hat keine Kontrolle über den Inhalt oder die Links der verlinkten Seiten.

